Shutterstock
Pancreatic cancer is one of the most aggressive and challenging cancers, often called a “silent disease” due to its lack of early symptoms. Despite advances in medical research, it remains a leading cause of cancer-related deaths worldwide. Understanding the risk factors, warning signs, and available treatment options can make a critical difference in outcomes. This guide delves into essential facts about pancreatic cancer, providing insight into prevention, early detection, and management. By increasing awareness and knowledge, we can work towards earlier diagnoses and improved survival rates.
What Is Pancreatic Cancer?

Shutterstock
Pancreatic cancer begins in the pancreas, a vital organ located behind the stomach that plays an essential role in digestion and blood sugar regulation. The disease develops when abnormal cells in the pancreas grow uncontrollably, often forming tumors. Pancreatic cancer can disrupt the body’s ability to process nutrients and regulate blood sugar levels. It is one of the most aggressive and deadly forms of cancer due to its often-silent progression.
Types of Pancreatic Cancer

Shutterstock
Pancreatic cancer comes in several forms, with the most common being adenocarcinoma, which arises in the ductal cells of the pancreas. Less common types include neuroendocrine tumors, which originate in hormone-producing cells and can behave differently than adenocarcinoma. The type of pancreatic cancer influences treatment options and outcomes significantly. Knowing the specific type is crucial for tailoring an effective treatment plan.
Silent Progression

Shutterstock
Pancreatic cancer is often referred to as a “silent disease” because symptoms usually do not appear until the cancer is in advanced stages. This delayed onset of noticeable signs makes it difficult to detect the disease early. By the time symptoms become apparent, the cancer has often spread to other parts of the body. This characteristic underscores the importance of regular check-ups, especially for those at higher risk.
Early Warning Signs

Shutterstock
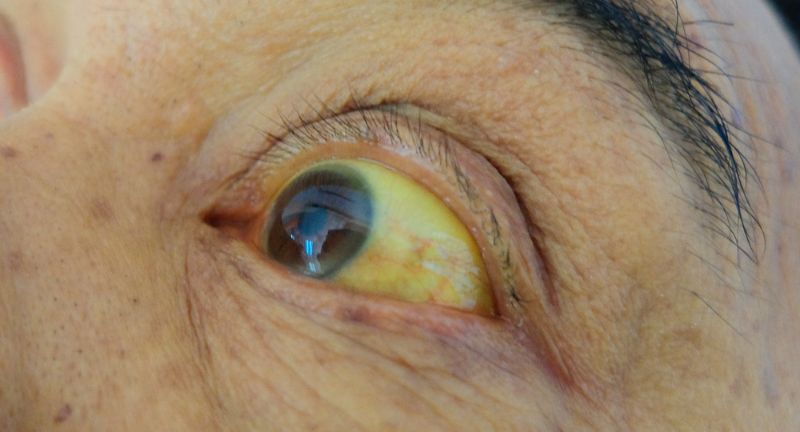
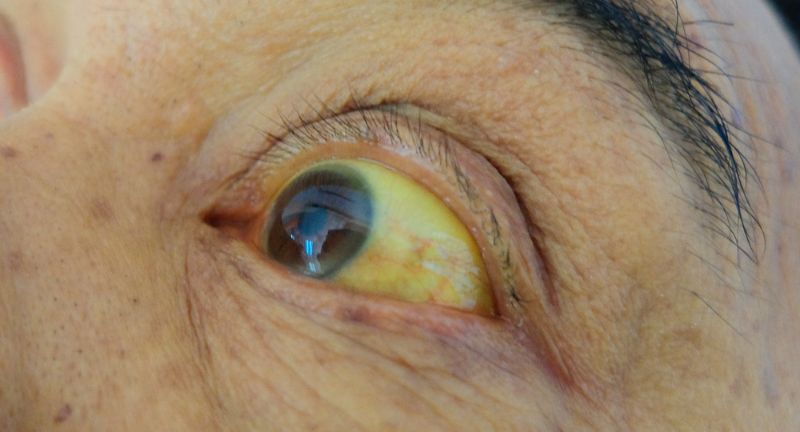
The early signs of pancreatic cancer are subtle and often mistaken for less severe issues. Symptoms include persistent abdominal or back pain, unexplained weight loss, and loss of appetite. Jaundice, characterized by yellowing of the skin and eyes, may also appear due to bile duct blockage. Recognizing and acting on these early warning signs can significantly improve the chances of successful treatment.
Jaundice as a Red Flag
Shutterstock
Jaundice, or the yellowing of the skin and eyes, is one of the most noticeable symptoms of pancreatic cancer. It often occurs when a tumor blocks the bile duct, causing a buildup of bilirubin in the body. Along with yellowing, patients may experience dark-colored urine and pale stools. This symptom should prompt immediate medical attention as it can indicate the presence of pancreatic cancer or other serious conditions.
Sudden Onset of Diabetes

Shutterstock
In some cases, pancreatic cancer can lead to the sudden onset of diabetes, especially in older adults without a prior history of the disease. The tumor’s effect on insulin-producing cells disrupts blood sugar regulation. Newly diagnosed diabetes may be an early sign of pancreatic cancer. If this occurs in conjunction with other symptoms, further investigation is warranted.
Risk Factors

Shutterstock
Several factors increase the risk of developing pancreatic cancer. Smoking is one of the most significant modifiable risk factors, doubling the likelihood of the disease. Chronic pancreatitis, family history of pancreatic cancer, and certain genetic syndromes also elevate the risk. Maintaining a healthy lifestyle and seeking regular medical evaluations are crucial for those with these risk factors.
Genetic Links

Shutterstock
Genetics play a significant role in pancreatic cancer, with mutations in genes like BRCA1 and BRCA2 increasing risk. Those with a family history of the disease or known genetic syndromes may benefit from genetic counseling and testing. Identifying genetic predispositions allows for closer monitoring and preventive strategies. Understanding one’s genetic makeup is a step toward early detection and intervention.
Age and Gender

Shutterstock
Pancreatic cancer primarily affects individuals over the age of 60, with cases rarely occurring in younger people. Men have a slightly higher risk of developing the disease compared to women, possibly due to lifestyle factors such as higher smoking rates. Age-related changes in the pancreas and cumulative exposure to risk factors contribute to this trend. Early recognition of symptoms in older adults is essential for timely diagnosis and treatment.
Diet and Lifestyle

Shutterstock
Diet and lifestyle choices play a significant role in pancreatic cancer risk. A diet high in red and processed meats and low in fruits and vegetables can increase susceptibility. Additionally, excessive alcohol consumption and obesity have been linked to chronic pancreatitis, a known risk factor for pancreatic cancer. Adopting a healthy diet and active lifestyle can help mitigate these risks.
Importance of Early Detection

Shutterstock
Early detection of pancreatic cancer significantly improves survival rates, yet it remains a challenge due to the disease’s subtle onset. Regular screenings for high-risk individuals, such as those with a family history or genetic predispositions, can aid in early diagnosis. Imaging techniques and blood tests are among the tools used for early detection. Timely intervention can make a critical difference in treatment success and quality of life.
Diagnostic Methods

Shutterstock
Several diagnostic methods are employed to detect pancreatic cancer effectively. Imaging tests such as CT and MRI scans help visualize tumors and their extent. Endoscopic ultrasound provides a closer view of the pancreas, often combined with tissue biopsy for confirmation. Blood tests, including markers like CA 19-9, are also used, though they are more effective for monitoring than initial detection.
Stages of Pancreatic Cancer

Shutterstock
Pancreatic cancer progresses through distinct stages, from stage 0 (confined to the pancreas) to stage IV (spread to distant organs). Each stage determines the treatment approach and prognosis. Early-stage cancers may be treated surgically, while advanced stages often require systemic therapies like chemotherapy. Understanding the staging is crucial for planning effective, individualized treatment strategies.
Treatment Options

Shutterstock
Treatment for pancreatic cancer varies depending on the stage and type of cancer. Surgery, such as the Whipple procedure, is often performed for early-stage cancers. Advanced cases typically require chemotherapy, radiation, or targeted therapies to slow progression and manage symptoms. Emerging treatments like immunotherapy are being explored through clinical trials, offering hope for future breakthroughs.
Survival Rates

Shutterstock
Pancreatic cancer has one of the lowest survival rates among cancers, with a five-year survival rate of approximately 10%. This is largely due to late-stage diagnoses when the disease has already spread. Early detection can dramatically improve outcomes, making awareness of symptoms and risk factors critical. Continued research and advancements in treatment are aimed at improving survival rates in the future.
Supportive Care

Shutterstock
Supportive care plays a vital role in managing pancreatic cancer, focusing on improving quality of life. Pain management, nutritional support, and emotional counseling are key components of this care. Palliative care specialists work alongside oncologists to address the physical and psychological challenges of the disease. Support groups and resources can also provide invaluable assistance to patients and their families.
Clinical Trials

Shutterstock
Clinical trials are essential for advancing pancreatic cancer treatment options. These studies explore innovative therapies, including targeted treatments and immunotherapies. Patients who participate in clinical trials gain access to cutting-edge treatments and contribute to scientific progress. Discussing trial opportunities with a healthcare provider can help determine if participation is a viable option.
The Role of Awareness
Shutterstock
Awareness is a powerful tool in the fight against pancreatic cancer. Understanding the risk factors and symptoms can lead to earlier diagnoses and better outcomes. Public education campaigns and advocacy groups are working to shed light on this disease. By increasing awareness, more lives can potentially be saved through early intervention.
Prevention Strategies

Shutterstock
While not all cases of pancreatic cancer can be prevented, certain lifestyle changes can reduce risk. Quitting smoking is one of the most impactful steps to take. Maintaining a healthy weight and eating a balanced diet rich in fruits, vegetables, and whole grains also play a role. Regular exercise and limiting alcohol consumption further enhance preventive measures.
When to See a Doctor

Shutterstock
Knowing when to seek medical attention is crucial for early detection of pancreatic cancer. Persistent symptoms such as jaundice, unexplained weight loss, or abdominal pain should not be ignored. If you have a family history of the disease or other risk factors, discussing preventive screenings with your doctor is essential. Prompt action can lead to earlier diagnosis and more effective treatment options.
Conclusion

Shutterstock
Pancreatic cancer remains a formidable health challenge, but knowledge and awareness are powerful tools in combating this disease. Recognizing the symptoms, understanding risk factors, and seeking timely medical advice can significantly improve outcomes. Advances in treatments and ongoing research continue to provide hope for patients and their families. By staying informed and proactive, individuals can play a crucial role in early detection and prevention. Together, we can work toward a future where pancreatic cancer is detected earlier and treated more effectively.